(this is the continuation from Part 1; in case you missed it, read it here)
Central Nervous System – The Olfactory System
Separating the olfactory epithelium from the brain is a very thin bone known as a cribriform plate, which is about as thick as a few pieces of paper stacked together. Sitting right above the cribriform plate is the olfactory bulb, which is actually part of the brain.
The first step in recognizing a smell is the activation of the olfactory epithelium. In humans, these cells are located in the olfactory clefts, at the highest part of the nasal cavity. The clefts have unique properties making them different than all other cells in nasal cavity. In fact, odorant-binding proteins have been discovered in the mucus covering the olfactory clefts that have not been found elsewhere.
A meta-analysis published in 2020 in the Asian Pacific Journal of Allergy and Immunology identified that 45% of all COVID-19 patients had olfactory dysfunction but up to 40% of those cases, the loss of smell was caused by congestion and swelling of the mucous membranes (i.e. like a bad head cold.) If this was the cause, symptoms usually resolve.
But when the olfactory clefts are damaged, the loss of smell does not seem to improve with the use of vasoconstrictors (nasal sprays), antibiotics, or steroids, and in fact, can be permanent. In spite of its regenerative capacity, neural olfactory dysfunction in humans often lasts for months to years and is sometimes permanent.
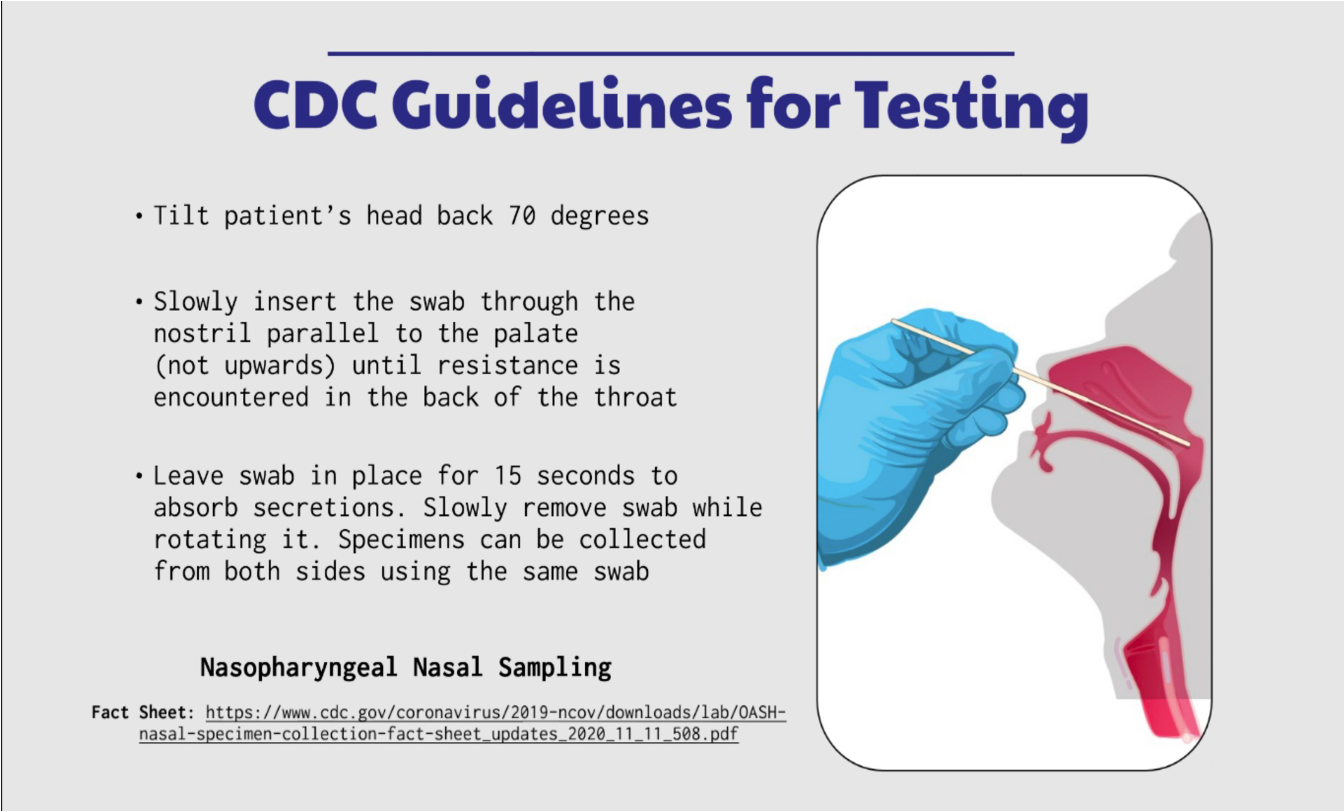
Researching and writing the above section made me wonder: how much intentional damage was done by the six-inch, deep nasal swab stabs with repeated PCR testing? What if the swab is inserted incorrectly, as in a “drive by” testing where you leaned out of the car and let someone jab you deep in the back of your nose?
What about those with long-haul anosmia?
In an attempt to answer that question, a study using specialized MRI imaging where the olfactory bulb could clearly be seen was undertaken. The study included 23 patients with persistent anosmia, lasting one to 14 months after they had otherwise recovered from the covid illness. All participants had previously had a PCR nasal swab to confirm COVID illness and at the time of the MRI, had documented anosmia at a local Smell and Taste Clinic.
A CT scan of the paranasal sinuses confirmed there was no evidence of mucus or congestion in ethmoid air cells or in the nasal passages that could have been the source of anosmia. All patients had abnormal MRIs, including partial (69.6%) and total (4.3%) olfactory cleft opacification (calcification). Their olfactory bulbs were reduced in size or had distorted shapes and they had a lost olfactory nerves.
Therefore, a plausible mechanism for long term anosmia may include direct damage to olfactory epithelium, olfactory bulb, and the olfactory cleft by the virus (spike protein), and/or damage to olfactory epithelium from inflammatory changes in surrounding tissues.
CONCLUSION: Our findings support the observations of olfactory cleft inflammation in COVID-19 anosmia.
AGAIN:
If the loss of smell is due to tissue inflammation, regeneration of the olfactory tissues can occur within a few weeks to a few months.
If the loss of smell is due to the destruction of the olfactory cleft, it can be permanent.
A French study, released in May 2021, actually concluded exactly that:
We demonstrated that multiple cell types within the olfactory neuroepithelium are infected at the time when loss of smell occurs... We hypothesize that persistence of COVID-19 associated loss of smell is linked to the inflammation caused by persistent infection.
In other words:
When the infection resolves, so does the inflammation.
When inflammation resolves, the tissues may be able to regenerate.
If the infection/spike protein causes destruction of the olfactory neuroepithelium or the olfactory cleft, regeneration may be very slow, or not at all.
What can be done?
As we have seen, there is evidence that COVID infection/inflammation - most likely associated with the spike protein - can wreak havoc throughout the entire olfactory apparatus, from the cilia to the olfactory cleft and beyond.
The sense of smell is not a ‘life-or-death’ organ like it is for lower animals, but we still depend on the ability to smell much more than we realize. One can gain an appreciation of the importance of smell by reflecting on how food becomes tasteless when you have a bad head cold. Long-term loss of smell has a significantly negative impact on the quality of life and sadly, the personal consequences remain overlooked by even the most well-informed health practitioners.
The neglect of our chemical senses is not new. Complaints of this nature are often overlooked in patients with Parkinson’s disease, acquired brain injury and cancer/chemotherapy. Because there are few helpful interventions, the psychological ramification are substantial. Food plays a huge part of our socialization and connectedness. When there is no taste or smell, the negative consequences are sometimes so strong that persons have confessed suicidal ideations and a general loss of interest in living.
As a result, people are desperate to find a solution. Unfortunately. many types of drugs, such as zinc preparations, Chinese medicine, topical and systemic steroids, vitamins, and metabolic agents have been tested, but none of them have been shown to be very effective in placebo-controlled randomized controlled trials.
Olfactory Training
One treatment that has had a modicum of success is called olfactory training, a method of stimulating the olfactory bulb and regenerating the overall olfactory system. The training is designed to expose the less/mal/non-functioning olfactory sensory neurons to odorants to improve their function.
In 2009, a study by Hummel et al. of 56 patients with severe anosmia were divided into two groups: one group did olfactory training with four odorants (phenylethyl alcohol (rose), eucalyptol (eucalyptus), citronellal (lemon), and eugenol (clove) twice a day for 12 weeks. The four training odorants were selected based on the classical classification of primary odors (odor prisms) proposed by Henning in 1916. The control group did not do the training.
Patients were advised to sniff the odors in the morning and in the evening for approximately 10 seconds through each nostril. Sniffin’ Sticks tests before and after the intervention period revealed that the training group showed better improvement of olfactory function, This clinical study is consistent with previous studies suggesting that the olfactory sense has to ability to change and recover.
Reading the actual study reveals that the overall improvement was only about 30%...but for most, that would be better than nothing.
Questions remained after the training:
Were the gains temporary or permanent?
Would the participants have gained more with ongoing training instead of ending at 12 weeks?
If they had stimulated the olfactory bulbs for more than 10 seconds each time, would the improvement increase?
Did training improve the overall sense of smell, or did it improve only to those oils used in the training?
Is dedicated daily training necessary or would occasional sniffing of the odors lead to the same result?
Since the time (2009), additional training protocols have been tested, including 16 weeks and 56 weeks of training and periodically changing the types of odors. Both appeared to enhance the success rate.
Overall, the essential oils of rose, lemon, cloves, and eucalyptus, the four types most often used in smell training, and have shown at least some positive effects for improving the sense of smell for patients with anosmia and/or hyposmia. All of these oils are available in our store - Here’s a direct link to the oils in the DrTenpenny.com store.
On page 17 of this highly informative 71 page paper is a table that has examples of odors and procedures used for olfactory training in mice. There is also a detailed section on stimulating the taste buds.
SUMMARY:
Currently, resolution persistent anosmia is not particularly hopeful. The longer it goes on, the more likely it is that the olfactory apparatus itself has been severely injured or destroyed. There are several promising novel therapeutic - but invasive - options under development, including tissue engineering and stem cell therapy.
I hope this gives some of you a few things to try, such as the olfactory training with essential oils. I took a deep dive into the medical literature about Covid-induced loss of smell, from the infection OR from the jab, hoping to find a lot of solutions. (it took more than 20 hours to research and write this article).
Sadly, what I found is much has been written about the mechanisms of this injury but very little emphasis has been placed on finding a resolution to what, for many, is a devastating problem.
(Have you seen it? I write a Sunday Substack called “Walking With God.” You can find it here.)
++++++++++
Additional References, in no particular order
Li, Wei, et al. “COVID-19, cilia, and smell.” The FEBS Journal 287. 2020; Pages 3672–3676.f
Trottier, Didier, et al. “Inflammatory Obstruction of the Olfactory Clefts and Olfactory Loss in Humans: A New Syndrome?” Chemical Senses, Volume 32, Issue 3, March 2007, Pages 285–292.
Kandemirli, Sedat Giray, et al. “Olfactory Bulb MRI and Paranasal Sinus CT Findings in Persistent COVID-19 Anosmia.” Academic Radiology, Vol. 28, No1, January 2021. Pgs 28–35.
Pedro Augusto Sampaio Rocha-Filho, MD, PhD ; Lara Voss, MD. “Persistent Headache and Persistent Anosmia Associated With COVID-19.” Headache 2020, 60:1797-1799.
Dias de Melo, Guilherme, et al. “COVID-19-related anosmia is associated with viral persistence and inflammation in human olfactory epithelium and brain infection in hamsters.” Translational Med. 10.1126/scitranslmed.abf8396 (2021).
Eliezer M, Hautefort C, Hamel A, et al. “Sudden and Complete Olfactory Loss of Function as a Possible Symptom of COVID-19.” JAMA Otolaryngol Head Neck Surg. 2020;146(7):674–675.
Lee, Yonghyun, et al. “Prevalence and Duration of Acute Loss of Smell or Taste in COVID-19 Patients.” J Korean Med Sci. 2020 May 11;35(18):e174
Saussez, Sven, et al. “Anosmia: an evolution of our understanding of its importance in COVID‑19 and what questions remain to be answered.” European Archives of Oto-Rhino-Laryngology (2021) 278:2187–2191
Genva, Manon, et al. “Is It Possible to Predict the Odor of a Molecule on the Basis of its Structure?” Int. J. Mol. Sci. 2019, 20, 3018; doi:10.3390/ijms20123018
Sharma, Anju, et al. “Sense of Smell: Structural, Functional, Mechanistic Advancements and Challenges in Human Olfactory Research.” Current Neuropharmacology, 2019, 17, 891-911
Najafloo, Raziyeh, et al. “Mechanism of Anosmia Caused by Symptoms of COVID-19 and Emerging Treatments.” ACSChem.Neurosci.2021,12,3795−3805
Miwa, Takaki, et al. “Clinical practice guidelines for the management of olfactory dysfunction.” Auris Nasus Larynx. Vol 46, Issue 5, p 653-62. October 1, 2019.
Hummel, Thomas, et al. “Effects of Olfactory Training in Patients with Olfactory Loss.” Laryngoscope, 119:496–499, 2009.
Iraon-Pour, Elham, et al. “Presentation with Anosmia and Ageusia: Possible Hidden Carriers of COVID-19.” Southern Medical Journal. Volume 113, Number 8, p 399-400. August 2020.
Butowt, Rafal, et al. “Anosmia in COVID-19: Underlying Mechanisms and Assessment of an Olfactory Route to Brain Infection.” The Neuroscientist 2021, Vol. 27(6) 582 –603.





Thank you so much for all of your research time. I love the smell therapy and using the essential oils. My sister is a chef and gardener and her loss of smell has impacted her in her profession. She said the only smell she has is of onions. But they don’t smell like they did. Have a blessed weekend. 💕
I see that Dr. Bryan Ardis claims that nicotine can be the solution to loss of taste and smell from the "vaccine" or the "virus".